Unstable Tachycardia: ACLS Course Chapter 15
ACLS unstable tachycardia is when the heart rate or rhythm is too fast (>100 beats/min). In persistent cases, it can lead to hypotension, acute heart failure, chest pain and possible signs of shock. An increase in heart rate causes less blood to be pumped through the systemic and pulmonary systems. Low blood flow will cause less oxygen to flow to the heart and brain and less oxygen to the heart can lead to Ischemia and MI. Unstable tachycardia is when the heart rate is too fast causing unstable conditions and symptoms caused by >150bpm, which is blood pressure per minute. Some symptoms may include:
- Hypotension
- Altered mental status
- Shock
- Chest pain or discomfort
- Acute heart failure
Unstable Tachycardia Video:
Unstable Tachycardia Rhythms Include:
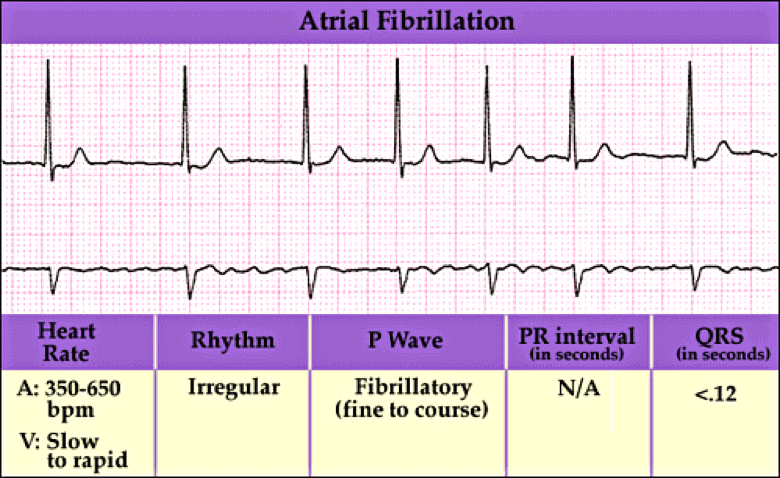
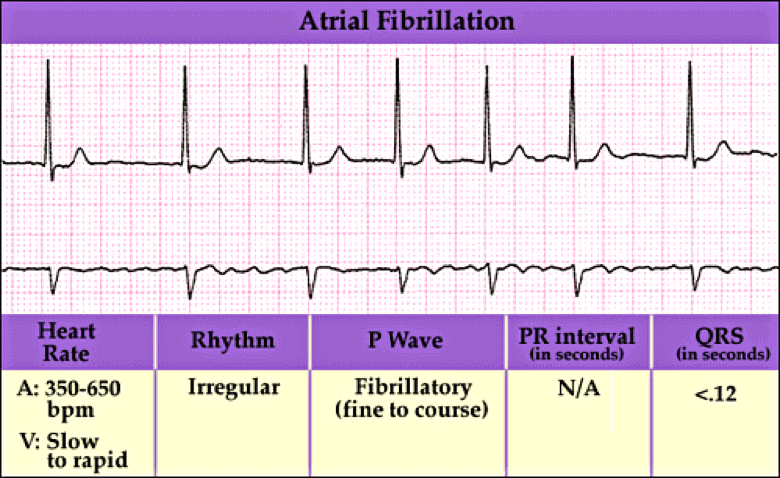
- Atrial fibrillation
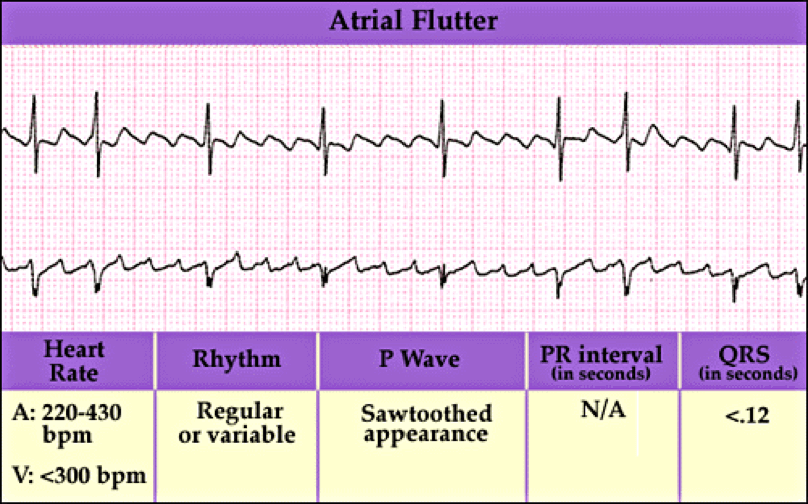
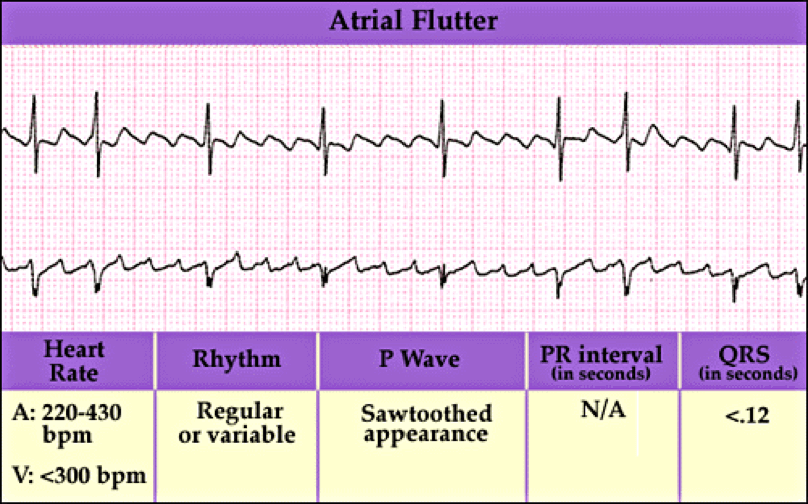
- Atrial flutter
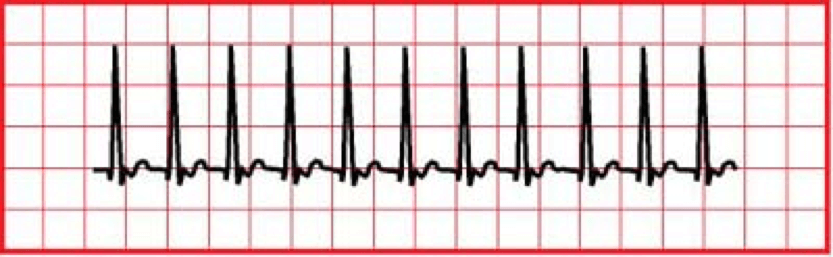
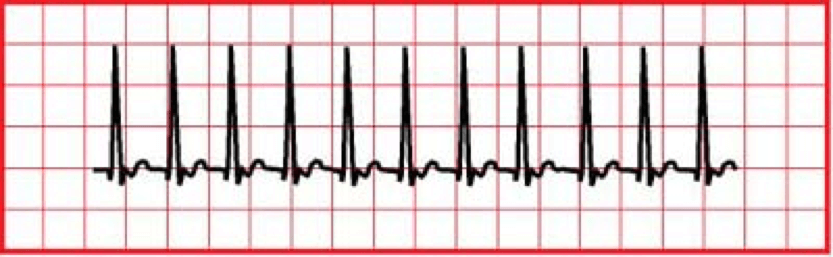
- SVT
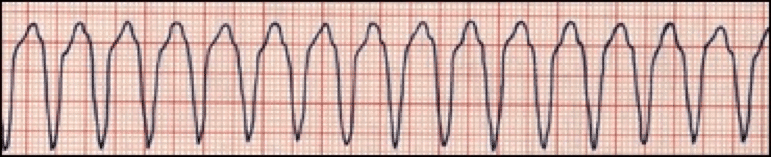
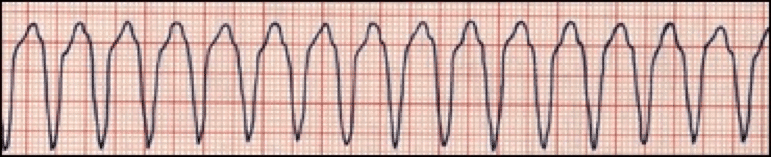
- Monomorphic VT
- Polymorphic VT
- Wide-Complex tachycardia of uncertain type
Atrial fibrillation is when the heart beats do not occur at the same intervals. It is known as the quivering of the muscles and involves both the atriums of the heart.
Atrial flutter is abnormal heart rhythm causing fast irregular heartbeat. Starts in the atrium and can lead to atrial fibrillation. Usually has a ‘saw-toothed’ appearance.
Supraventricular Tachycardia (SVT) is a rapid and narrow heartbeat that starts in the atria or AV node.
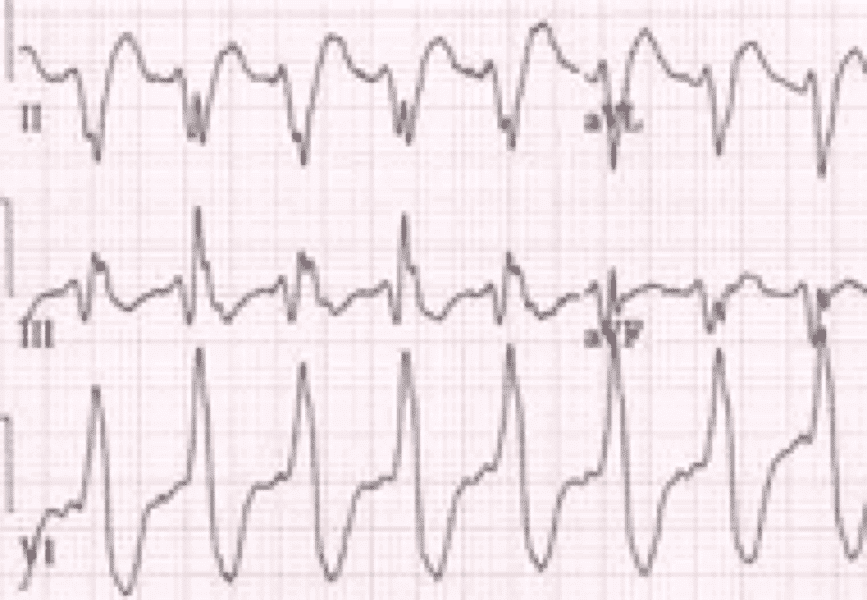
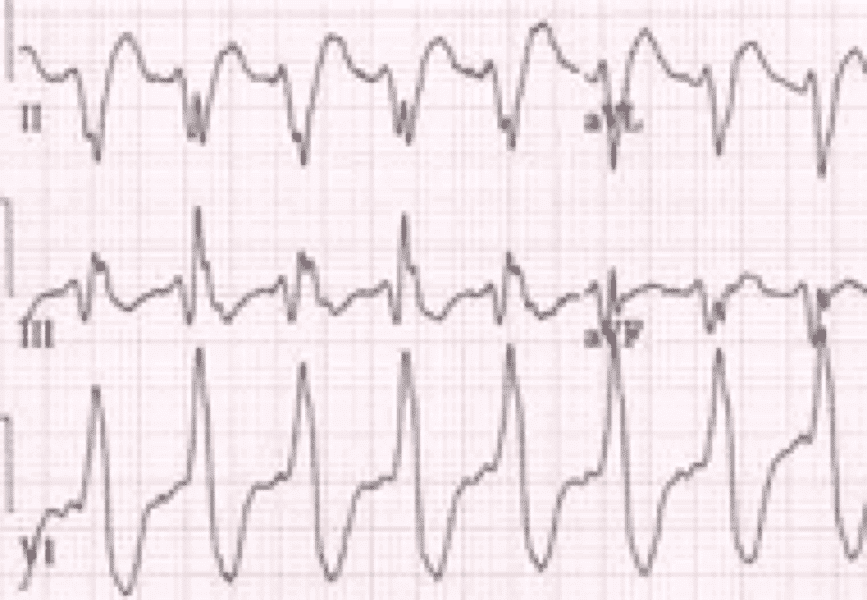
Monomorphic VT is heart rate of >150 bpm but all QRS look the same.
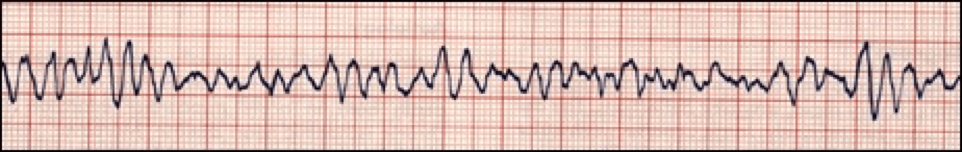
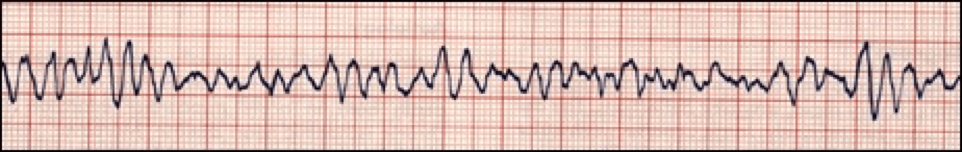
Polymorphic VT is when different areas in the ventricles fire fast, uncoordinated impulses.
Wide-complex tachycardia is due to ventricular tachycardia or SVT with wide QRS complex (at least 0.12 seconds).
Scenario: A 45 year old patient arrives to the hospital with chest pain and palpitations. As the nurse was obtaining medical history and checking vital signs the patient faints for a few minutes.
Unstable Tachycardia Rhythm Assessment:
- Check for responsiveness – Tap and shout, “Are you alright?” and look at chest for movement. Check carotid pulse and note there is pulse and breathing
- Put the patient on a monitor and identify Tachycardia (>100 beats/min)
- Call the doctor on duty
Unstable Tachycardia Rhythm Interventions:
- Maintain airway
- Help with breathing and give oxygen if hypoxemic and monitor O2 saturation
- Monitor BP and HR and conduct a 12-lead ECG and diagnose
- Check for persistent tachyarrhythmia
Unstable Tachycardia Rhythm Management:
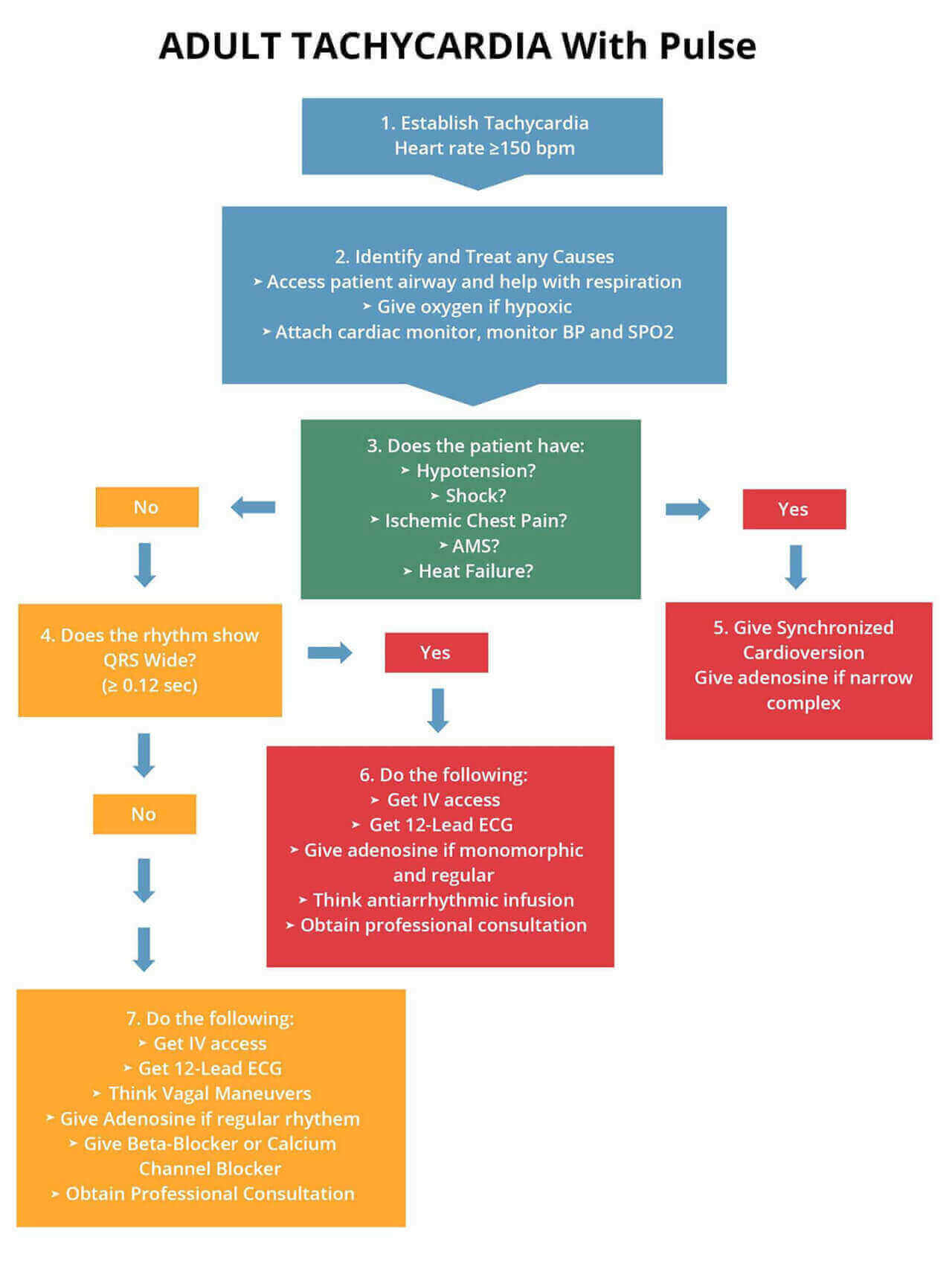
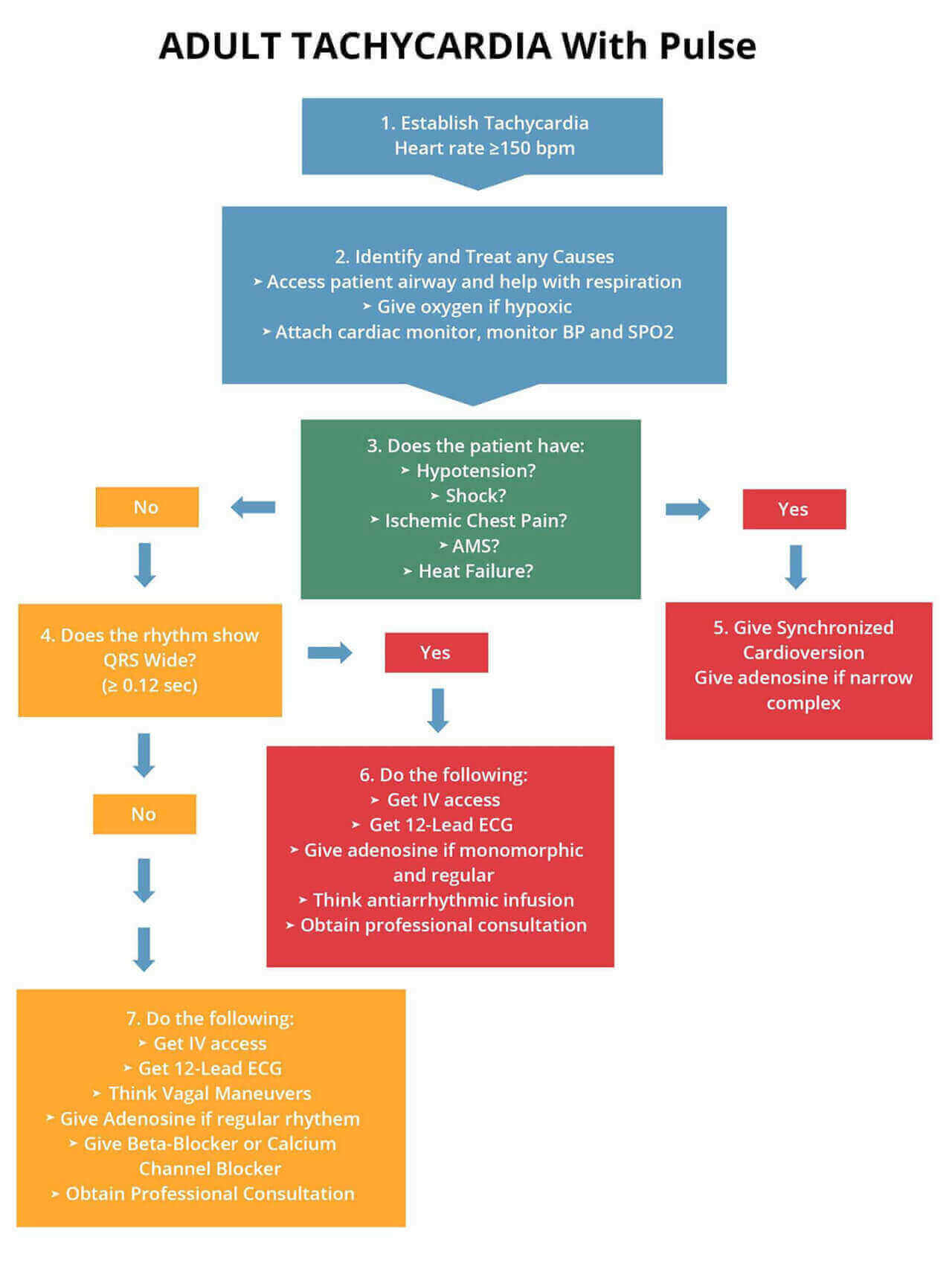
- If persistent tachyarrhythmia initiates synchronized cardioversion
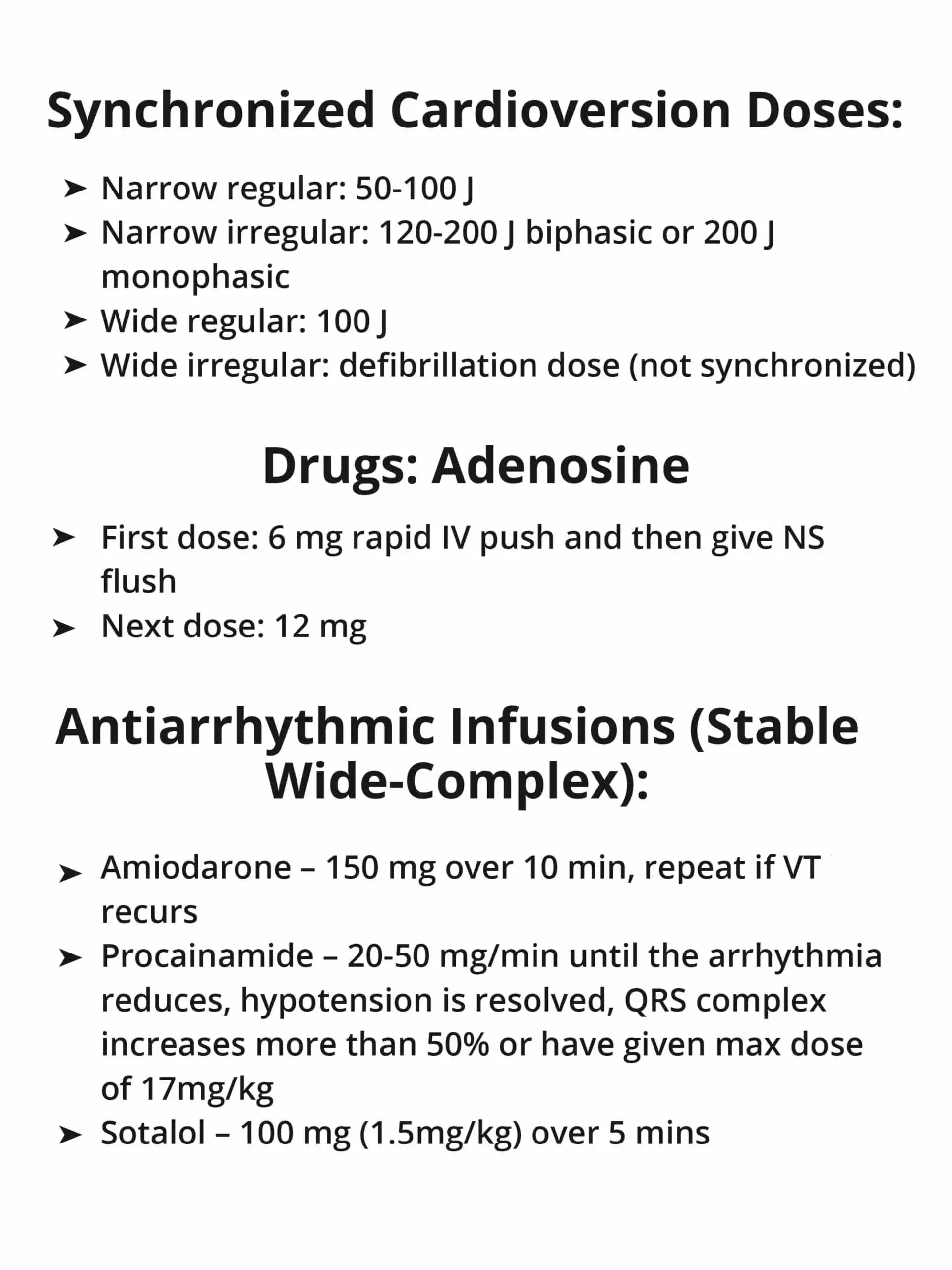
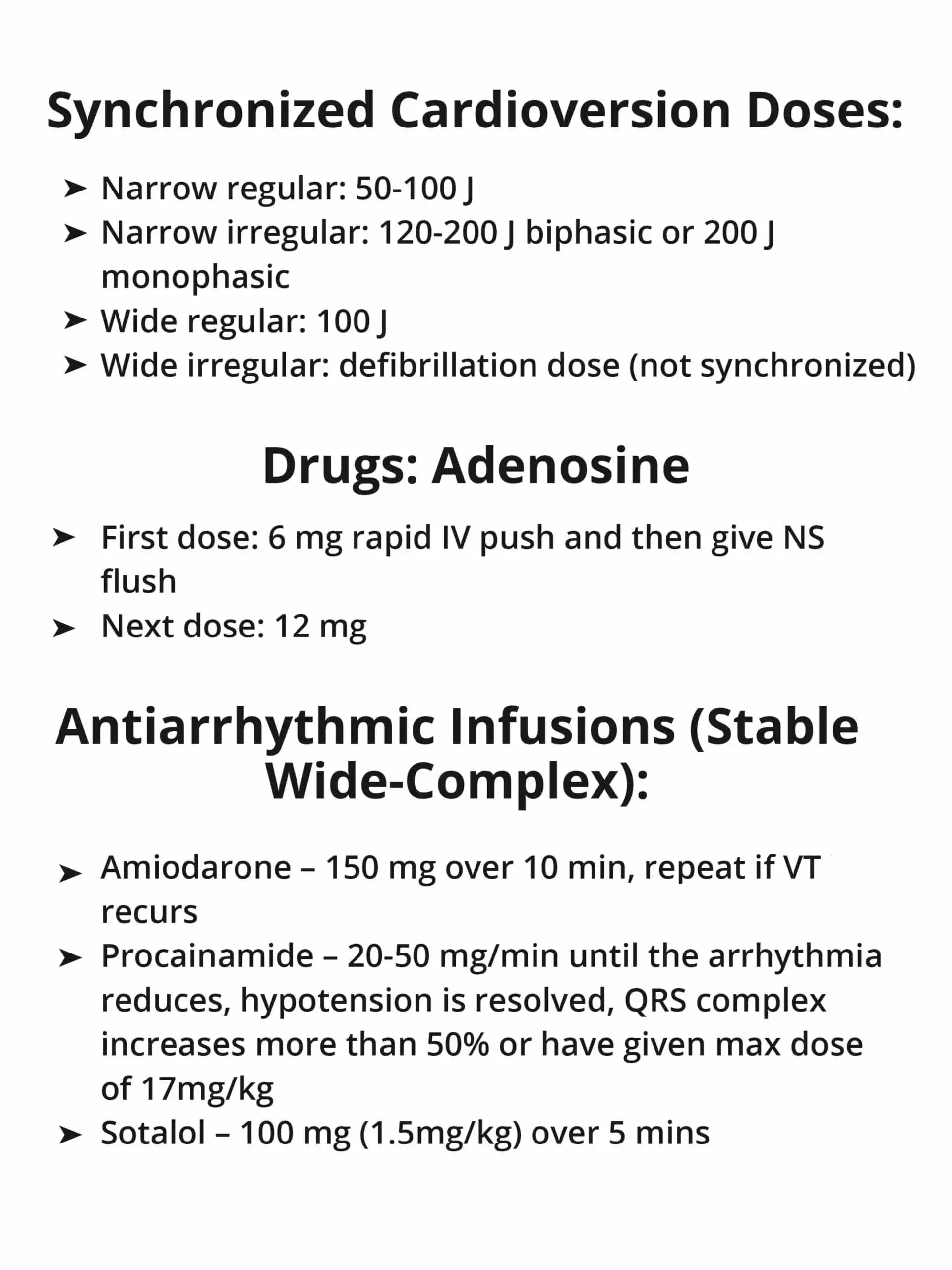
- Narrow regular 50-100 J
- Narrow irregular 120-200 J biphasic and 200 J monophasic
- Wide regular 100 J
- Wide irregular defibrillation dose
- Administer Adenosine IV dose 6mg rapid IV push with NS flush and 12 mg for second dose
- If not persistent tachyarrhythmia and if wide QRS ≥12 seconds, then obtain IV access and 12-lead ECG
- Administer Adenosine if monomorphic
- Administer antiarrhythmic infusion (Procainamide, Amiodarone, Sotalol)
- If not irregular wide QRS consider vagal maneuvers, adenosine, beta blockers, calcium channel blockers
The following is an algorithm showing management of unstable tachycardia in detail:
Cardioversion
Synchronized cardioversion is used during unstable tachycardia, but there may be times when unsynchronized cardioversion will need to be used.
Synchronized cardioversion needs to be used with:
- Unstable SVT
- Unstable atrial fibrillation
- Unstable atrial flutter
- Unstable regular monomorphic tachycardia with a pulse
Unsynchronized cardioversion needs to be used with:
- No pulse
- Critical issues – patient going into cardiac arrest
- Patient in monomorphic or polymorphic VT
- Patient at risk of going into arrest
Energy in Joules used during cardioversion:
| Rhythm |
First Dose (Monophasic Defibrillator) |
| Unstable atrial fibrillation |
200 J |
| Unstable Monomorphic VT |
100 J |
| Other unstable SVT, Atrial Flutter |
200 J |
| Unstable polymorphic VT (irregular form & rate) |
Use like VF with high-energy shock (360J) |
| How to Give Synchronized Cardioversion |
Anesthetize patient unless they are crashing or unstable
- Turn on the defibrillator
- Put the leads on the patient and ensure the rhythm is on the monitor. Put on the adhesive electrode pads on the patient
- Push the SYNC button to get to the synchronized mode
- Ensure the markers are on the R wave – this shows that the sync mode is on
- Pick the correct energy level
- Ensure everyone is clear – “Stand clear, charging defibrillator!”
- Push the charge button
- Again clear patient – “Everyone Clear!”
- Push the shock button
- Check rhythm to see if tachycardia is still present. If tachycardia is persistent, increase energy level slowly
- Press SYNC button again to activate the sync mode
|
Learning Outcomes:
You have completed Chapter XV. Now you should be able to:
- Recognize the types of ECG rhythms associated with Tachycardia
- Apply the Adult Tachycardia Algorithm in Unstable Tachycardia
- Understand the signs & symptoms of Tachycardia
- Understand synchronized and unsynchronized cardioversion