Chapter 6: Shock
Pediatric shock is a serious condition that occurs when there is inadequate supply of oxygen to meet the needs of the tissues. Lack of oxygen to the peripheral tissues cause the tissues to stop functioning properly and is a leading cause of morbidity and mortality in the pediatric population. There are 4 types of shock that occurs in children:
- Hypovolemic shock – inadequate blood volume or oxygen-carrying capacity
- Distributive shock – inappropriately distributed blood volume
- Cardiogenic shock – impairment of heart contractility
- Obstructive shock – obstructed blood flow
PALS Course By American HealthCare Academy Video:
Hypovolemic Shock
The most common cause of shock in children is hypovolemia and is mostly due to fluid loss. Hypovolemia can be identified by decreased preload, increased or normal contractility and increased afterload. The following are the causes of hypovolemic shock:
| Causes of Hypovolemic Shock |
|
|
|
|
- Decreased fluid consumption
|
|
|
|
|
|
|
|
|
| Signs of Hypovolemic Shock |
|
|
|
|
|
|
- Weak or absent peripheral pulses
|
- Normal or weak central pulses
|
|
|
|
|
|
|
|
|
Management of Hypovolemic Shock
Nonhemorrhagic Hypovolemia
The key to management of nonhemorrhagic hypovolemia in children is the infusion and retention of fluids. Proper and timely administration of fluids is crucial in treating hypovolemic shock and can quickly lead to recovery. Infusion of 20 ml/kg boluses of isotonic crystalloid will be effective to treat a child with hypovolemic shock and up to 3 boluses can be given if the patient doesn’t improve.
Hemorrhagic Hypovolemic Shock
For hemorrhagic shock start with fast infusion of isotonic crystalloid in boluses of 20 mL/kg and give up to 3 boluses for a total of 60 mL/kg. For every 1 mL of blood loss, it is important to supplement 3 mL of crystalloid for the initial treatment. If the patient remains unresponsive consider Packet Red Blood Cells (PRBCs) transfusion in 10 mL/kg boluses.
There are no pharmacological interventions that are effective for either hemorrhagic or nonhemmorrhagic hypovolemic shock. Therapy includes fluid dosage, identifying the cause of volume loss and correcting metabolic imbalance.
Distributive Shock
Distributive shock occurs when there is improper distribution of blood volume and there is decreased organ and tissue perfusion. Distributive shock can be identified as normal or decreased preload, normal or decreased contractility and afterload that is variable. There are 3 types of distributive shock:
- Septic shock
- Anaphylactic shock
- Neurogenic shock
The 2 key treatment options for distributive shock are: restoration of hemodynamic stability and identification and control of infection.
PALS Training By American HealthCare Academy Video:
Septic Shock
Septic shock causes a decrease in tissue perfusion and oxygen due to infection by certain organisms or endotoxins. Septic shock can be identified by decreased preload, normal to decreased contractility and an afterload that is variable. The following are signs of septic shock:
| Signs of Septic Shock |
|
|
|
|
- Elevated or decreased WBC count
|
|
|
|
|
|
|
|
|
|
|
|
|
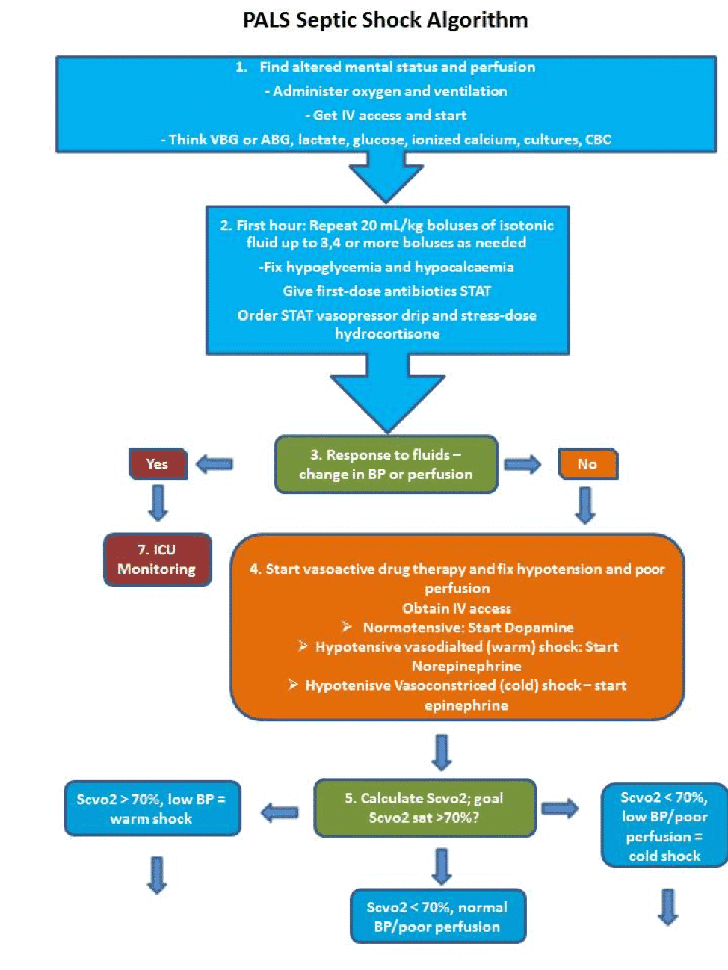
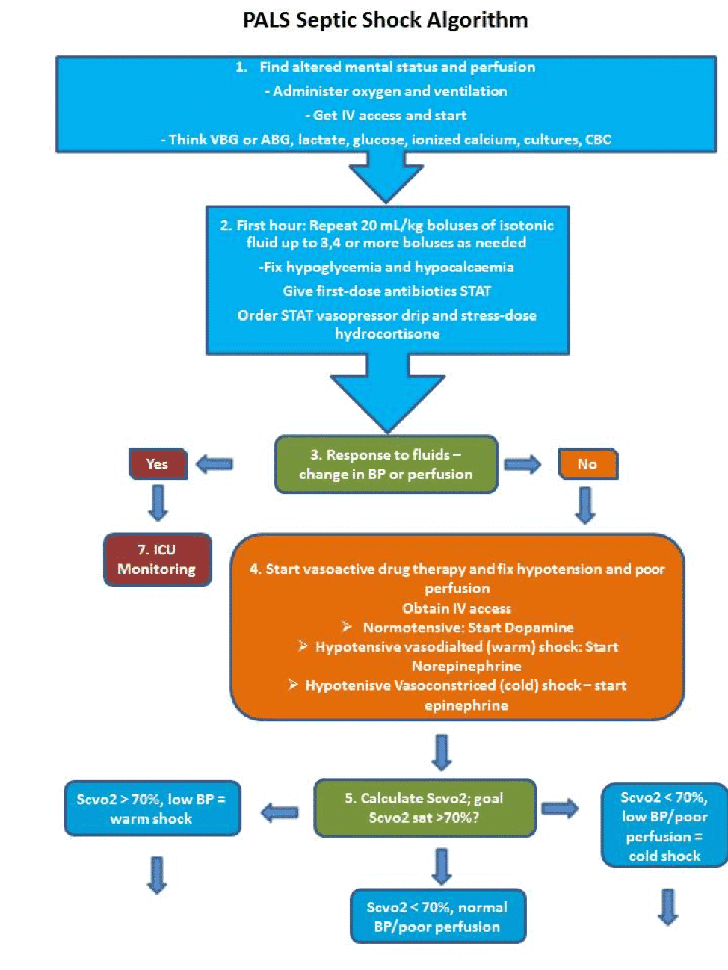
Management of Septic Shock
The following description shows the proper methods in treating septic shock:
- Give oxygen and support ventilation
- Obtain vascular access and obtain labs
- Within the first hour administer repeated doses of 20 mL/kg boluses of isotonic fluid
- Correct hypoglycemia and hypocalcaemia
- Give the first dose of antibiotics
- Order STAT vasopressor drip and stress-dose hydrocortisone
- If there is no response to the fluid treatment start with vasoactive drug treatment
- For Normotensive start with dopamine
- For Hypotensive vasodilated (warm) shock start with norepinephrine
- For Hypotensive vasoconstricted (cold) shock start with epinephrine
- Evaluate the Scvo2 (N = sat >70%
- If Scvo2 <70% with normal BP and poor perfusion – transfuse to Hgb>10 g/dL and think of giving milrinone or nitroprusside and dobutamine
- If Scvo2 <70% with low BP and poor perfusion with cold shock – transfuse to Hgb>10 g/dL and give epinephrine or dobutamimne+norepinephrine
- If Scvo2 >70% with low BP and warm shock give additional fluid boluses and norepinephrine with/without vasopressin
- If there is response to fluid therapy transfer to ICU and continue monitoring
The following is an algorithm showing the management of septic shock in pediatric patient:
Anaphylactic Shock
Anaphylactic shock results in vasodilation and low blood pressure with bronchoconstriction causing the child to stop breathing immediatly. Anaphylaxis occurs due to reaction to a certain good, drug, toxin, vaccine, plant, poison or antigen. Signs and symptoms of this shock include:
| Signs and Symptoms of Anaphylactic Shock |
|
|
|
|
|
|
|
|
|
|
- Swelling of face, lips and tongue
|
- Respiratory distress = wheezing or stridor
|
|
|
|
|
Management of Anaphylactic Shock
The primary goal in the treatment of anaphylaxis is to target problems associated with bronchoconstriction and vasodilation.
- Give oxygen and support ventilation
- Obtain vascular access and obtain labs
- Adminiter a dose of 20 mL/kg boluses of isotonic cystalloid bolus over 5 to 20 minutes and repeat to restore blood pressure and tissue perfusion
- Conduct ancillary studies
- Administer the following medications for rapid recovery
- Epinephrine – IM epi or epi by autoinjector — a second dose of epi injection may be needed after 10-15 mins at a low dose of < 0.05 mcg/kg/min
- Albuterol for bronchospasm – 4 to 8 puffs every 20 minutes or 2.5-5 mg/dose every 20 minutes for nebulizer
- Antihistamine- H1 blocker Diphenhydramine – 1 to 2 mg/kg IV/IO/IM every 4 to 6 hours with max dose of 50 mg
- Corticosteroid- Methylprednisolone – 2 mg/kg IV/IO/IM for max dose of 80 mg
- Continue treatment and monitoring until child is out of shock
- Give oxygen and support ventilation
- Obtain vascular access and obtain labs
- Within the first hour administer repeated doses of 20 mL/kg boluses of isotonic fluid
Neurogenic Shock
Disruption of the autonomic pathway of the spinal cord due to head or spine injury results in hypotension, bradycardia and loss of sympathetic nervous system signals to the smooth muscle in the vessel walls.
Management of Neurogenic Shock
- Give oxygen and support ventilation
- Obtain vascular access and obtain labs
- Adminiter a dose of 20 mL/kg boluses of isotonic cystalloid bolus over 5 to 20 minutes and repeat to restore blood pressure and tissue perfusion
- Conduct ancillary studies
- Position the child head down to improve venous return
- Consider using vasopressors such as norepinephrine or epinephrine for hypotension
- Epinephrine – 0.1 to 1 mcg/kg/min
or
- Norepinephrine – .05 – .1 mcg/kg/min
- Provide cooling or warming as needed
Cardiogenic Shock
Cardiogenic shock results when the ventricles of the heart fail to function properly and there is inadequate circulation of blood throughout the body. Cardiogenic shock can be identified by a variable preload, decreased contractility and an increased afterload. The causes and signs of cardiogenic shock include:
| Cause of Cardiogenic Shock |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Signs of Cardiogenic Shock |
|
|
- Increased respiratory effort due to pulmonary edema
|
|
|
- Weak or absent peripheral pulses
|
|
|
- Jugular venous distention
|
|
|
|
|
|
|
|
|
|
|
PALS Course By American HealthCare Academy Video:
Management of Cardiogenic Shock
- Give oxygen and support ventilation
- Obtain vascular access and obtain labs
- Administer a dose of 5 to 10 mL/kg boluses of isotonic cystalloid bolus slowly over 10 to 20 minutes PRN
- Conduct ancillary studies
- Obtain assess for pulmonary edema
- Administer the following medications:
- Catecholamine – Dobutamine – if necessary
- Catecholamine – Dopamine – if necessary
- Vasodilator – Nitroglycerin – 0.25 to 0.5 µg/kg per minute IV/IO and increase to 0.5 to 1 µg/kg per minute every 3 to 5 minutes PRN
- Vasodilator – Sodium Nitroprusside – 1 to 8 µg/kg per minute IV/IO for <40 kg child and 0.1 to 5 µg/kg per minute IV/IO for >40 kg child
- These may be required:
- Milrinone – Loading dose of 50 mcg/kg for 1 to 60 mins, followed by 0.25 to 0.75 mcg/kg/min
- Nitrogylcerin – 1 to 5 mcg/kg/min
- Nitroprusside initial dose 0.3 to 1 mcg/kg/min
Obstructive Shock
Obstructive shock results when there is obstruction of the great vessels of the heart and results in impaired cardiac output. Proper management of obstructive shock includes correction of cardiac output and tissue perfusion. There are 4 types of obstructive shock:
- Cardiac tamponade
- Tension pneumothorax
- Ductal-dependant congenital heart lesions
- Massive pulmonary embolism
PALS Certification by American HealthCare Academy Video:
Cardiac Tamponade
Cardiac tamponade occurs when there is accumulation of fluid, blood, pus or air in the pericardium and is usually due chest trauma, hypothyroidism, pericarditis, cardiac surgery, cancer and myocardial rupture. Some signs and symptoms of cardiac tamponade include:
- Muffled or diminished heart sounds
- Pulsus pardoxus – decrease in systolic pressure
- Distended neck veins
- Decreased venous return
- Impaired ventricular filling
- Decreased cardiac output
Management of Cardiac Tamponade
The key to management of cardiac tamponade is the removal of fluid from the pericardial sac (pericardiocentesis) and proper administration of fluids for quick improvement of the child.
Tension Pneumothorax
Tension pneumothorax is accumulation of gal or air in the pleural cavity and can be caused by a tear from injured lung tissue, or chest trauma. Some signs of tension pneumothorax include:
| Signs and Symptoms of Tension Pneumothorax |
- Decreased or diminished breath sounds on the affected side
|
|
|
- Hyperresonance on the affected side
|
- Tracheal deviation toward contralateral side
|
- Deterioration in perfusion
|
- Tachycardia to bradycardia (quick)
|
|
|
|
|
|
|
|
|
Management of Tension Pneumothorax
Treatment of tension pneumothorax includes needle decompression and thoracotomy of chest tube placement. The physician or trained professional should insert an 18-20 gauge- over- the needle catheter on the top of the child’s 3rd rib for successful dissemination of air.
Ductal-Dependent Lesions
Ductal dependent heart lesions are birth defects of the heart that are seen in the first weeks of life. The ductal dependent lesions include ductal dependent for pulmonary blood flow and one for systemic blood flow. The ductal lesions for pulmonary blood flow are seen without shock but with cyanosis in the child. The left ventricular outflow tract obstructive lesion is seen with shock in the first 2 weeks of life when the patent ductus arterisous closes. Signs of ductal dependent for systemic blood flow include:
| Signs of Ductal-Dependent Lesions |
|
|
- Preductal versus postductal differential blood pressure
|
- Preductal versus postductal differential cyanosis
|
- Absence of femoral pulses
|
- Decreased in mental status
|
|
|
|
|
- Rapid progressive deterioration in systemic perfusion
|
Management of Ductal-Dependent Lesions
Management of ductal dependent lesions is by administration of prostaglandin E1 which restores ductal patency by vasodilation. Other management techniques include support by oxygenation, administration of inotropic agents to improve contractility, fluid administration to fix cardiac output and correction of metabolic imbalances.